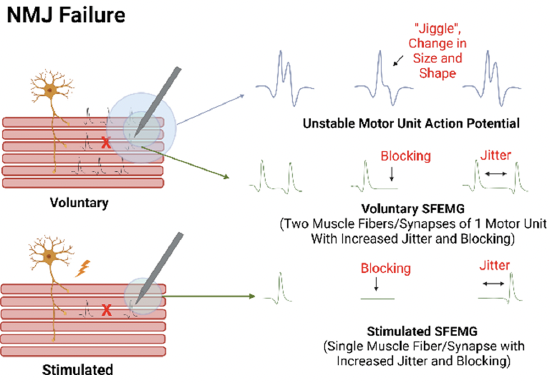
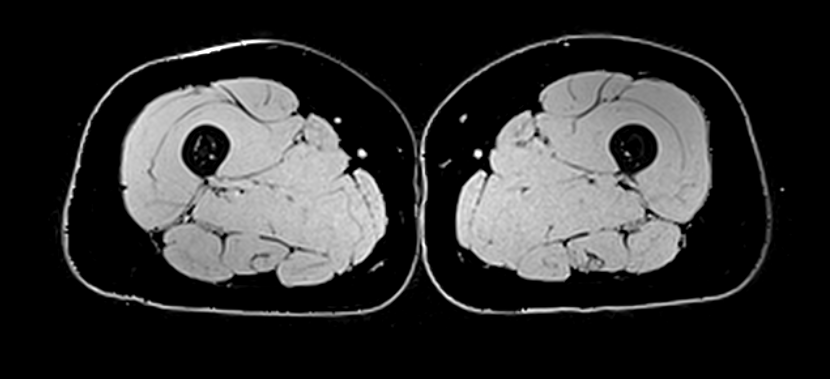
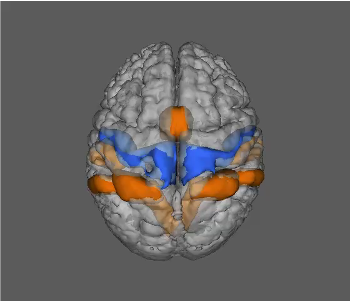
The overall goal of our laboratory's research is to improve the diagnosis, treatment, and prevention of sarcopenia, frailty, and osteoporosis. This work ranges from more basic studies on the neuromuscular mechanisms of age-related impairments in muscle function and mobility, to the development of innovative technologies and approaches for improving the diagnosis of sarcopenia and osteoporosis, to conducting clinical trials on novel drugs (e.g., myostatin-inhibitors, skeletal muscle calcium sensitizers, and neurotherapeutic agents), exercise interventions, and nutritional supplements. As such, our work is centrally focused on ‘translational physiology’, as it sits at the intersection of the bench and bedside. Overall, this work seeks to improve the diagnosis, treatment, and prevention of sarcopenia, frailty, and osteoporosis, and the research across the various foci has an overarching aim of developing interventions that ultimately extend the health span and promote healthy aging.
The overall goal of our laboratory's research is to improve the diagnosis, treatment, and prevention of sarcopenia, frailty, and osteoporosis. This work ranges from more basic studies on the neuromuscular mechanisms of age-related impairments in muscle function and mobility, to the development of innovative technologies and approaches for improving the diagnosis of sarcopenia and osteoporosis, to conducting clinical trials on novel drugs (e.g., myostatin-inhibitors, skeletal muscle calcium sensitizers, and neurotherapeutic agents), exercise interventions, and nutritional supplements. As such, our work is centrally focused on ‘translational physiology’, as it sits at the intersection of the bench and bedside. Overall, this work seeks to improve the diagnosis, treatment, and prevention of sarcopenia, frailty, and osteoporosis, and the research across the various foci has an overarching aim of developing interventions that ultimately extend the health span and promote healthy aging.
Looking for science-based tips for healthy aging? Please visit the NIH MedLine Plus Magazine.
Want to watch an hour long seminar about the research? If so, view a lecture Dr. Clark delivered in the fall of 2024.